What started as a career in psychiatric nursing has since catapulted me into the world of HCCs. Having worked on both sides, I can honestly say I love my hybrid career of nurse and coder. I’ve gained some perspective after 12 years of HCC experience and one year with KIWI-TEK. Here is some HCC information I thought our readers might enjoy.
Why do HCCs matter?
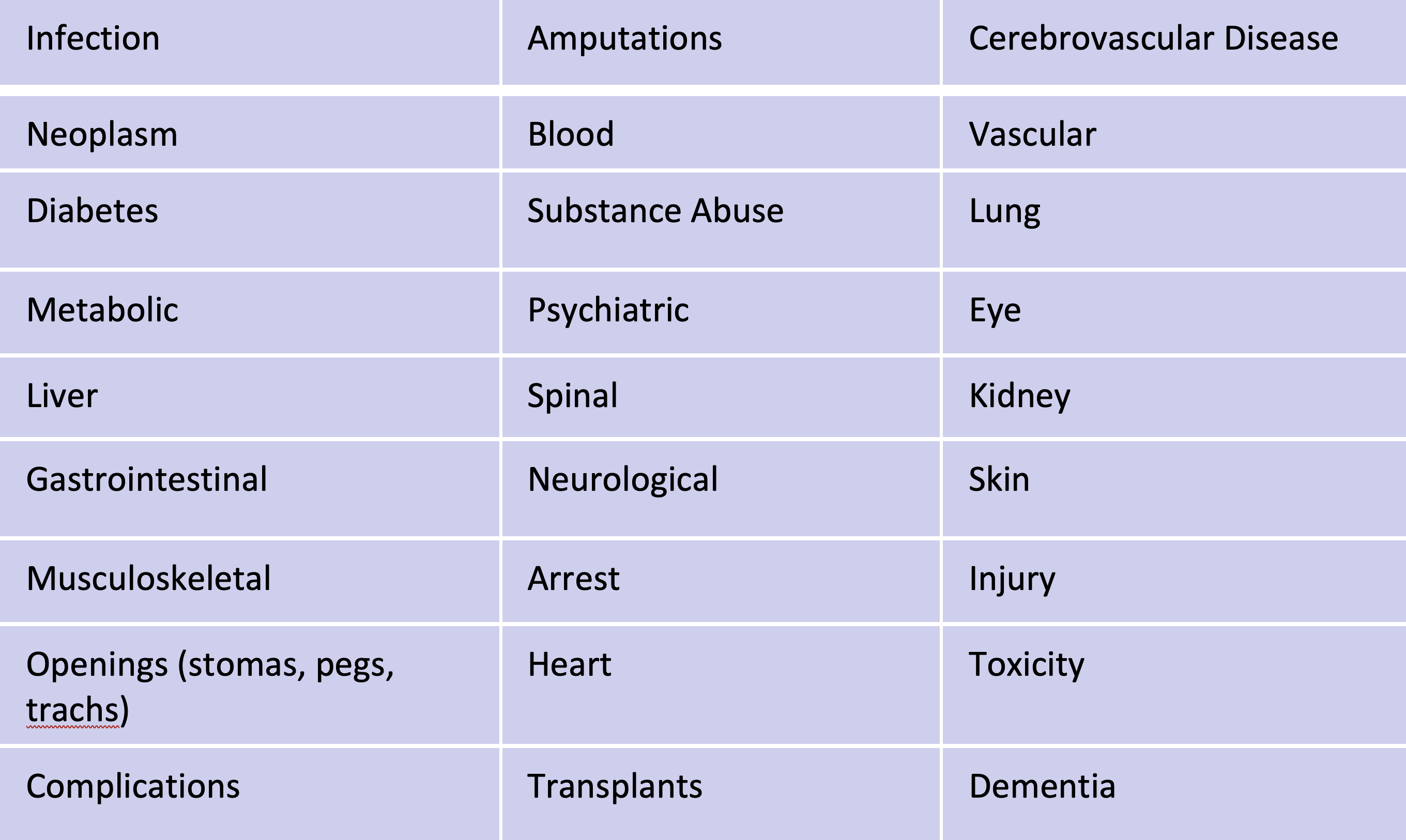
Out of tens of thousands of ICD-10 codes, there are 87 groups of Hierarchical Condition Categories (HCCs). HCC coding is a risk-adjustment model originally designed to estimate future health care costs for patients. HCCs are linked to 8,800 chronic diagnoses that can be more severe and costly.
Categories are diagnosis groupings based on:
The goal on the patient care side is to take Medicare Advantage patients who we know have severe diagnoses, manage them well and get them on the right treatment plans. The goal on the financial side is to be sure reimbursement is properly captured for providers who treat severe diagnoses.
Why are more and more organizations focusing their efforts on HCC capture?
Medicare Advantage (MA) plans signed up another 2.3 million beneficiaries for the 2022 coverage year, with the program now making up 45% of all Medicare enrollment, a new study found.
MA patients continue to be a growing part of a healthcare organizations’ payer mix going forward. Expanding CDI efforts into the outpatient setting with a focus on HCCs is essential for risk adjustment models.
There’s a lot of work to be done by coding and documentation professionals and HCC auditors.
OIG warns to document with caution
A key Department of Health and Human Services (HHS) watchdog warned that it plans to root out fraud and waste in coding, which has become a major source of criticism in the MA space.
What triggers questions from the auditors are key outliers in such data like chart reviews or physician claims.
“We are trying to find areas in the data analytics that pop out as aberrations. We are looking at what is happening in cases and what are we hearing about on the ground. We are taking all of that data and information and trying to find places where unusual events are occurring.” – Megan Tinker, assistant inspector general for OIG
Here are some red flags the OIG looks for:
- Diagnoses on a physician claim without a corresponding inpatient claim
- Diagnoses typically treated with a medication but, when compared against prescription data, don’t indicate a prescription being provided
- Cancer diagnoses serious enough that they should be accompanied by claims for surgical, radiation or chemotherapy within six months
Good documentation matters
There’s a two-pronged approach in my HCC Auditor role.
I conduct HCC sweeps, where I sweep the chart to look at the previous year’s notes – progress, consult, labs, Rx and more. I review HCCs already documented that need to be brought into the current year.
I also find new HCCs during chart reviews around 1-2 weeks before a patient is seen. My sticky notes for clinicians in the EHR might include something like, “In this consult note, you never captured this diagnosis. When the patient comes in for the next face-to-face visit can you assess to increase RAF score?”
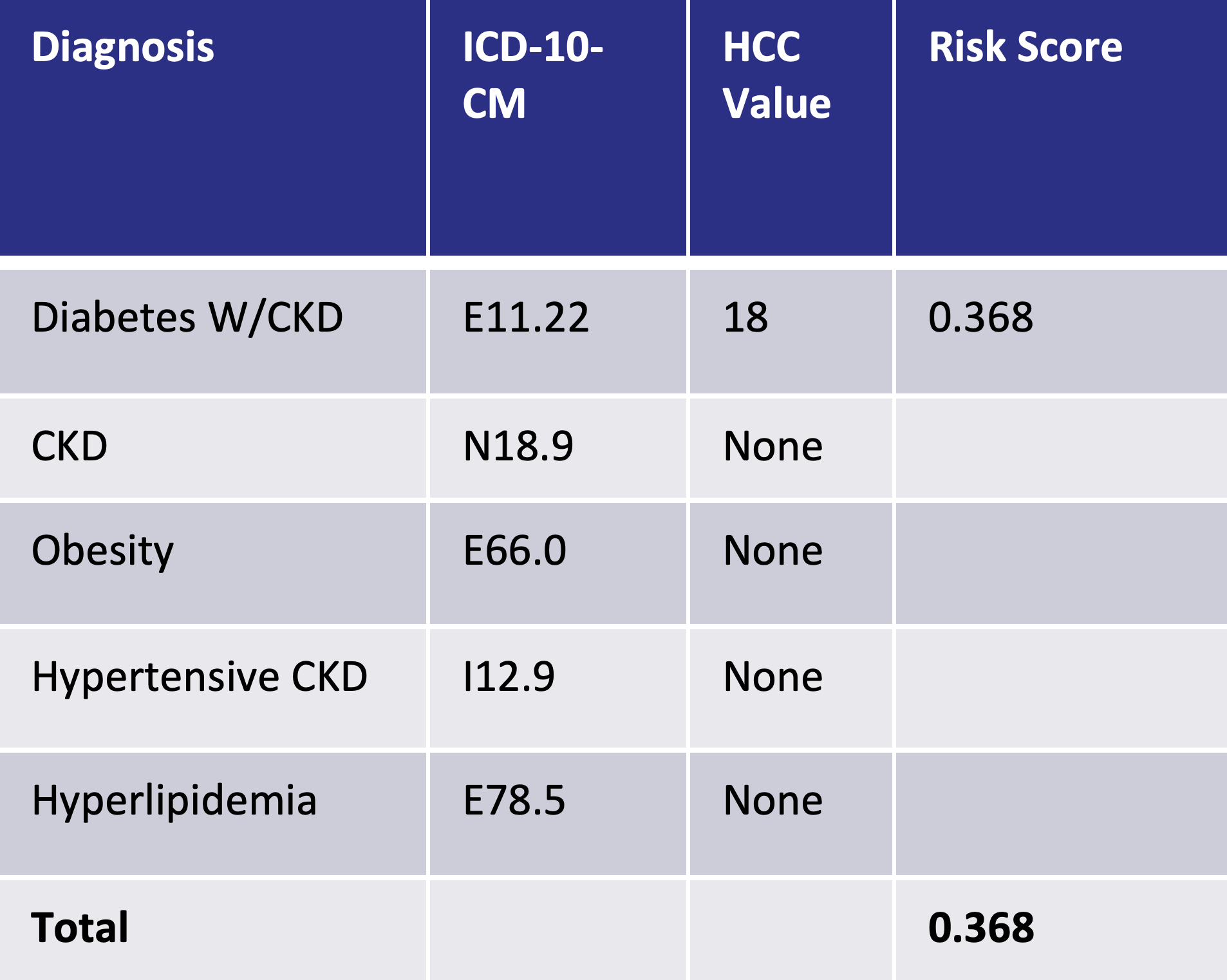
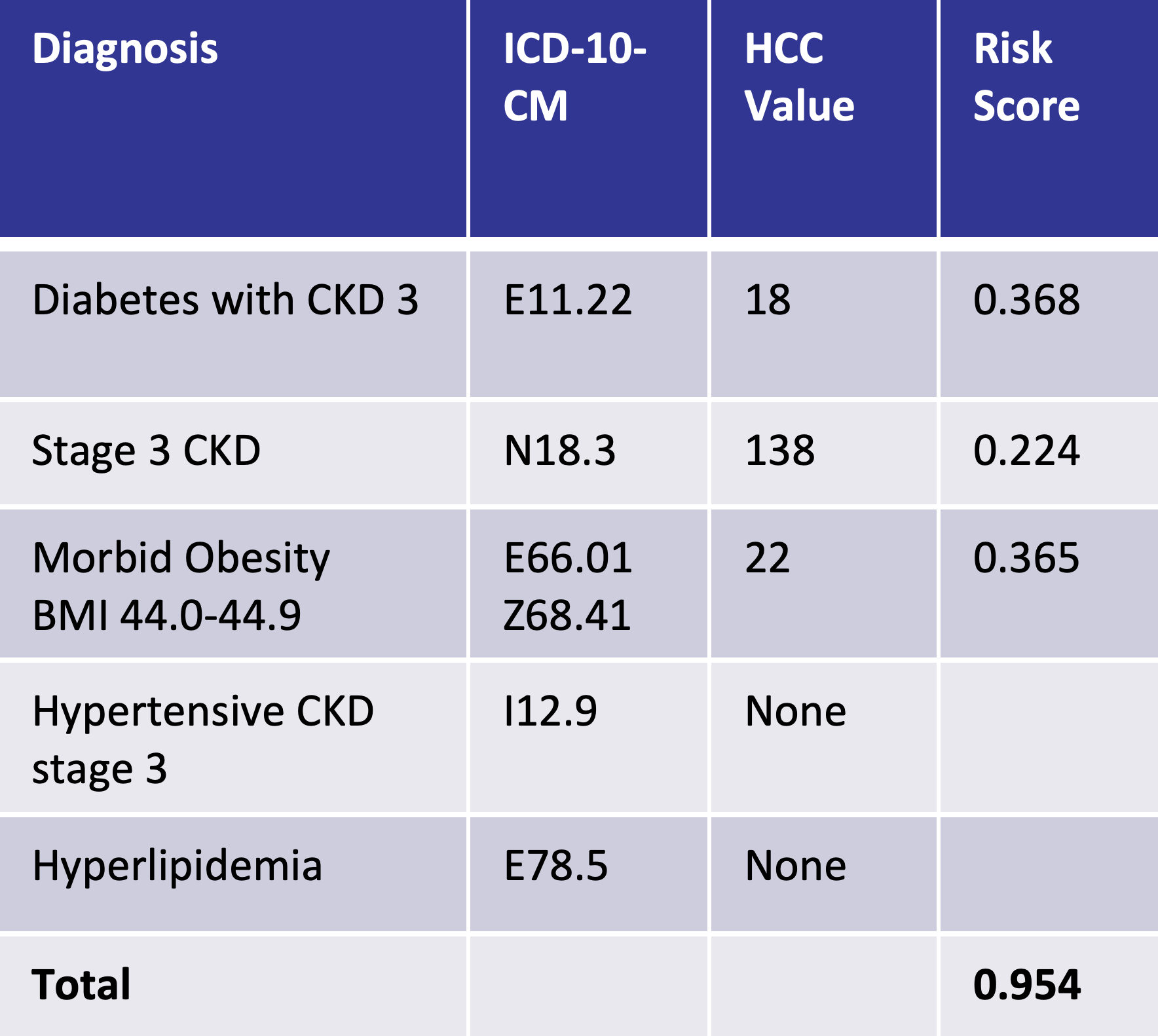
An example this can be seen below, with poor documentation on the left and the impact of good documentation on the right. With improved documentation, the risk score improves from 0.368 to 0.954:
Improve chronic condition documentation
KIWI-TEK can help you improve coding accuracy and compliance to demonstrate expected cost of care. To learn more visit https://kiwi-tek.com/consultation/
