Coding Changes in Patient Volume
In an effort to control the spread of the pandemic and to focus on COVID-19 patients, providers were directed in March to cancel elective surgeries and all other non-urgent patient visits. Prior to that time, patient volume by type of visit was fairly predictable, which helped with staff planning as well as forecasting revenue cycle metrics.
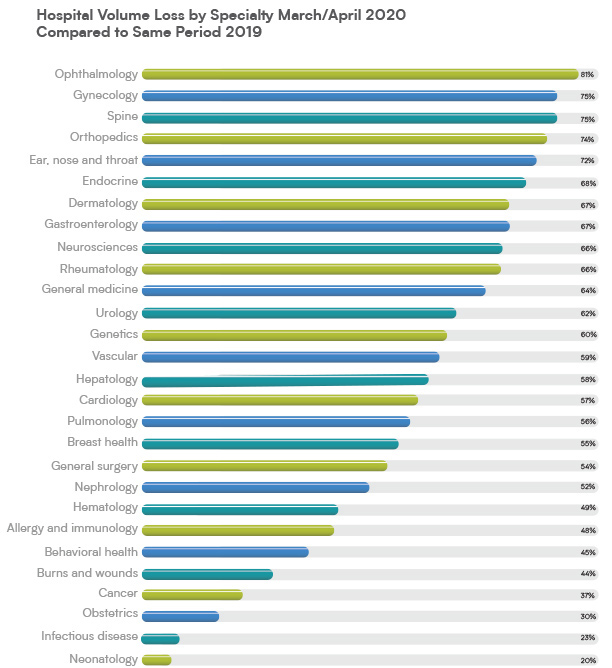
Very quickly, patient volumes for same-day surgeries, ED visits and other outpatient services were drastically reduced. Here are examples of volume loss by service line for 2 million patient visits and 228 hospitals analyzed by Strata Decision Technology:
Imaging and lab services started to recover from the pandemic by May 1, but hospital volume recovery still has a way to go as patients continue to avoid inpatient and ED care.
How does the decrease by service line correlate to revenue? Some experts predict an average loss of $1.4B in daily hospital revenue due to the decline in patient volume.
Coding professionals who coded those patient types for years suddenly had no work. Many experienced layoffs, furloughs, a reduction in hours or a leave of absence with the option to return.
Coding Changes in Patient Type
As patient volume dipped severely, a flood of telemedicine encounters came to HIM, with no one trained to code them. The proper education was released and coders were trained, with no time to spare. In a matter of weeks, HIM management reorganized and cross-trained their staff to provide the necessary resources for coding telemedicine visits, training on the new codes, assisting in a CDI role for the new documentation challenges, and auditing to monitor adherence to the new coding guidance.
One significant change in patient encounter types worth noting is remote patient monitoring (RPM). According to Gloryanne Bryant, RHIA, CDIP, CCS, CCDS, AHIMA-Approved ICD-10-CM/PCS Trainer, RPM has been very helpful for ongoing treatment during the COVID-19 pandemic. It enables clinicians to remotely monitor temperature and pulmonary function, blood pressure and other appropriate physiology for changes in a patient’s disease and symptom progression, using digitally connected, non-invasive devices such as sensors for body temperature or thermometers, pulse oximeters and home blood pressure monitors.
Lessons Learned
What did this sudden change in patient volume and patient type teach us as an industry?
Flexibility. You never know when you will need to learn new code sets, accommodate new patient types or reorganize and cross-train your coding staff. We talked about the importance of changing our perspective in a previous blog post. The pandemic may be the shock needed to produce a long-overdue review and possible change in coding strategy for healthcare providers’ revenue cycle operations.
Patience. You can’t resolve sudden, drastic changes to your revenue cycle overnight. Tough decisions had to be made in HIM staffing to survive the crisis. Let’s keep in mind that furloughs are temporary and the patient volume will come back. The HIM community has a history of resiliency and innovative problem-solving, having undergone many industry changes since its inception in 1928. The coronavirus challenge is one for the books! But patience and hard work have always gotten us through difficult times.
Teamwork. Suddenly, disparate departments in health systems had to collaborate more closely than ever before. Clinicians, registration, HIM, IT, HR and billing had to adjust to new, drastic changes in patient volume to ensure the integrity of the revenue cycle. Will this newfound cohesive teamwork across departmental silos continue? No one knows for sure. But hopefully the concept of collaboration and constant communication among teammates will be sustained over the long term.
Be sure to check out our previous post on documentation and coding for new patient encounters.
The Legacy of COVID-19
Impact on HIM now and in the future